The monkeypox outbreak: What we learned so far, and what could be better
Penn experts, including Annenberg professor Andy Tan, discuss the response to the monkeypox outbreak and how the public can be better informed for the future.
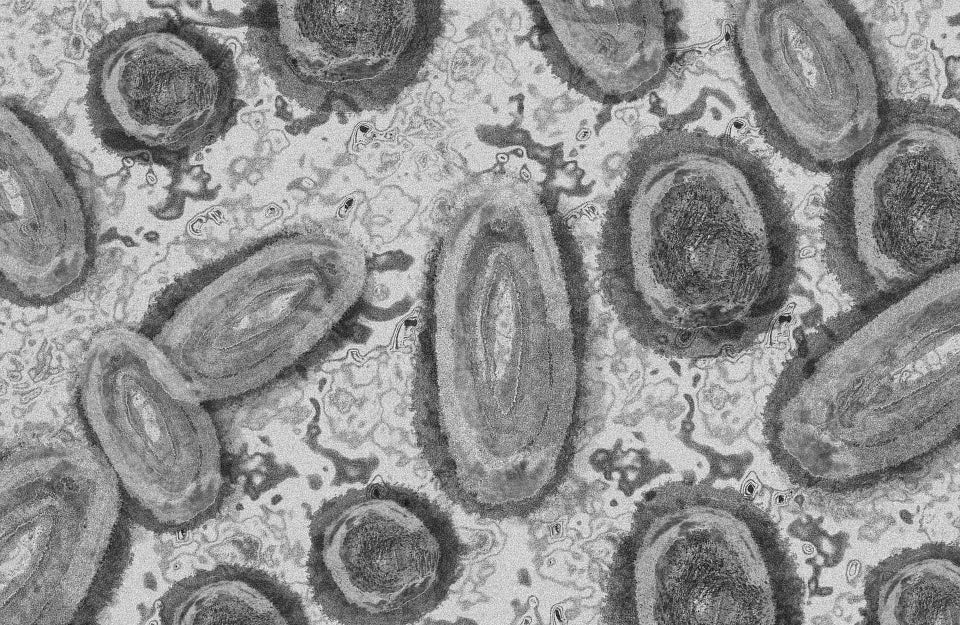
Photo Credit: Gerd Altmann / Pixabay
Whether because of vaccination, behavioral changes, or a spread-limiting mode of transmission, one takeaway is evident: The monkeypox outbreak has not exploded in the way it could have. Cases in the U.S. have declined to a few dozen per day, a drop-off from 440 cases per day in August. Demographically, the virus is still spreading primarily among men who have sex with men (MSM), mostly dodging the fear in the early fall of spillover into the broader public through daycare facilities and college campuses.
And yet, the response to the outbreak has been far from perfect.
As the outbreak emerged in early summer, news broke that 20 million doses of Bavarian Nordic’s JYNNEOS vaccine for smallpox and monkeypox, what is currently used to vaccinate high-risk individuals, had expired as part of a longer term plan to develop and purchase a freeze-dried version of the vaccine, a form that would have a more stable shelf life. The vaccines were purchased as part of the Strategic National Stockpile (SNS), created after the anthrax scare in 2001; the SNS is maintained by the U.S. Department of Health and Human Services (HHS) and the Centers for Disease Control and Prevention (CDC). Because of the expirations, only 1.4 million liquid-frozen doses were available for use when the outbreak began in the U.S., drawing from an order made in early 2020.
When demand spiked during the summer and doses were in short supply, the Food and Drug Administration (FDA) issued an emergency use authorization to administer the JYNNEOS vaccine intradermally, meaning it would be injected between layers of skin rather than under the skin, thus requiring a smaller dose and creating five total doses per vial. The catch: Intradermal injections require more skill to administer, and data on the effectiveness of cutting the dose and applying intradermally is limited to a single study conducted in immunocompetent people. Moreover, the method also causes an itchy red mark at the site of injection, and for some has caused scarring—further feeding concerns of stigma.
And despite vaccination rates climbing, the outbreak remains in a fluid position: On Tuesday, Nov. 2, HHS Secretary Xavier Becerra renewed the public health emergency for the outbreak, and reasons for the decline in cases are still up for debate.
The state of the outbreak
Stuart Isaacs, an associate professor of medicine at the Perelman School of Medicine, who studies poxviruses, says he’s hopeful the downward swing will continue, but it’s still too early to celebrate an end to the outbreak.
“I think it’s too early to see where this is going to go, because I think the decreasing cases is largely due to people doing less risky behavior, but that’s only going to last a certain amount of time,” Isaacs says. “There’s also a whole concern about other populations getting this and then having an upswing again of a whole new [group of] people who have been less educated about risk.”
In short, Isaacs explains that initial data collected on effectiveness of the vaccine so far is susceptible to bias. It’s possible, he says, that people who have been vaccinated tend to take more precautions than those who have not been.
What he does find encouraging, however, is that the virus does not seem to be spreading within households. While some children have been infected, the numbers barely make a dent in the total number of cases, indicating, he says, that it does not spread efficiently outside of intimate or sexual relations. There has also been some evidence in recent weeks that the virus does not exist in abundance in saliva or blood, but does exist in abundance around the anus and genitals—in addition to where any skin lesions might exist.
He says it’s also reassuring that, according to the CDC, more than a million doses have been administered, including second doses. It implies there is at least a baseline immunity, Isaacs says, that may not prevent all monkeypox disease but should provide protection and lead to less severe disease among those vaccinated.
In general, Isaacs says this point can get lost in public health messaging—similar to what happened with the COVID-19 vaccines.
“I think a lot of the messaging of the COVID vaccines were really bad at the beginning because they were presenting amazing data four weeks after the second dose, when you had the highest level of neutralizing antibodies—but that was a false expectation,” he says. “And similarly, vaccines that protected against smallpox did not provide lifelong protection from smallpox, but likely provided protection from severe disease and death, which is pretty amazing.”
Isaacs says he was surprised to learn that the SNS did not stock enough of the JYNNEOS vaccine, but does see the value in a plan to dry the vaccine. In the past decade, the SNS purchased raw materials to compile the vaccine in a freeze-dried manner, which is an ongoing process that still needs FDA approval.
“One of the beauties of the poxvirus is they’re so hearty they can be dried down to a powder,” he adds.
Public health communication and ethics
An additional hurdle in the monkeypox vaccine rollout is the sensitive nature of the target demographic for the vaccines, given the LGBTQ community’s historical—and in many ways still present—experience with HIV and stigma. Much anxiety existed in the early weeks of the outbreak around overly associating the virus to MSM circles or stressing temporary behavioral change too much.
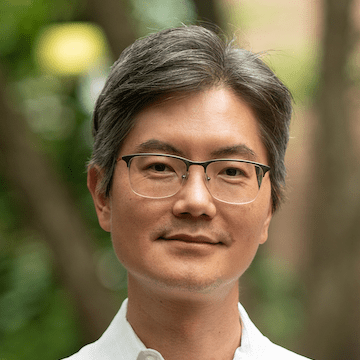
There’s also a risk, says Andy Tan, an associate professor of communication at the Annenberg School for Communication and director of the Health Communication & Equity Lab, that emphasizing one community over another in messaging would give the broader population a false sense of security. It’s a public health needle that’s difficult to thread.
“But at the same time,” Tan says, “[it’s important to] not overtly send out fear-based types of messaging that puts people at relatively lower risk of getting the disease too anxious or worried about getting infected and potentially using resources not intended for them.”
This is all happening, of course, in context of the COVID-19 pandemic, and similarities certainly do exist between the two outbreaks and their responses.
“Time is of the essence in making sure accurate information gets out to the public and specific populations at risk, and that they take the necessary precautions available to them at that point in time,” says Tan, citing one similarity. “But another similarity would be uncertainty, given the novelty of the coronavirus back in 2020, and more recently with monkeypox, which is not a new virus but the fact that it’s now transmitted through human interaction is fairly new.
“[We’re] getting that information out in a space of uncertainty.”
Despite challenges during the JYNNEOS vaccination rollout, including ongoing racial inequities and a shortage of doses in early months, a nationally representative Annenberg Public Policy Center survey conducted in August and released in September indicates rapid growth in knowledge about monkeypox. Sixty-one percent of those surveyed reported knowing a vaccine exists, up from 34 percent the prior month; 63 percent knew that MSM are at a higher risk of infection, up from 33 percent in July; and 84 percent said they know monkeypox spreads through close contact with an infected person, up from 69 percent in July.
Still, only 35 percent considered themselves “somewhat or very familiar with the disease” in the survey. And while vaccine uptake in minority populations—particularly Black and Latino ones—has increased in recent weeks, according to CDC data, they remain disproportionately low compared to white people.
The takeaway: Public health messaging is working, but with room for improvement.
Tan advocates for selecting communication channels very specifically to reach MSM, using trusted messengers to deliver information. Philadelphia, for example, has worked with the Mazzoni Center and the William Way LGBT Community Center for vaccination drives, and recent efforts have attempted to deliver vaccine messaging at nightclubs. In Atlanta, the vaccine was advertised at a Black gay pride festival.
Tan calls this type of messaging “mavenism,” which involves identifying individuals who are notable—ranging from a politician to a barbershop owner—to serve as trusted messengers in a community where those individuals have a high degree of trust. In part, it’s a lesson learned from the COVID-19 pandemic: Tan says he’s worked with Philadelphia parents and caregivers who’ve vaccinated their young children—who initially had reservations—to serve as messengers for other parents or caregivers who are unsure about vaccinating their children. He says the efforts have had some success, generated enthusiasm, and is an example of how a peer-to-peer community-led form of messaging shouldn’t be underestimated, even with the availability of mass media alternatives.
An issue that remains for monkeypox, however, is messaging in rural communities and cities where there are fewer of these specific LGBTQ channels to work with.
“We [in Philadelphia] are in a unique situation here where we have infrastructure that’s been built up over time. It doesn’t happen overnight, and so in other contexts, geographic locations, where there isn’t such a health center [like Mazzoni] available or infrastructure for disseminating this critical information to specific populations, there’s a huge challenge. Who do we rely on at that point?” Tan says. “That’s an open question.”
Harald Schmidt, an assistant professor of medical ethics and health policy, who teaches a course this semester on public health ethics, echoes that community-led efforts appear to be where vaccination drives have had the most success.
“Where the COVID vaccine rollout has worked well is where people did work with communities and recognized the sensitivity around the nature of the vaccine, the need for it, and that that differed across populations,” Schmidt says. “That, as well as lessons from HIV, should be combined with knowledge from public health workers. That’s an imperative.”
Schmidt adds that we seem to find ourselves in a moment of awakening regarding equity and the differential impact of infectious diseases, whether it’s COVID-19 or monkeypox.
“That’s the forward-looking mission, as we’re coming to the end of this monkeypox [outbreak]: We want to learn, as we have with COVID, what we can do next time where it hasn’t worked as effectively as it could have?” he says, adding, “Where are the equity coordinators? And how do you recognize social and ethnic equity?”
The mission is not to expect perfection in a response, Schmidt says, but to keep learning and adjusting. That might mean better record-keeping, better pay for stretched-thin public health departments, new positions in public health, or re-examining dose allocations.
“With all these pandemics, you can’t prepare for each and every detail that will wash over us, but the fact is, once it’s there, it’s [often] ‘Oh, just limit the damage, let’s think on our feet.’ And you think, ‘Hang on, shouldn’t we have better data and conceptual reference points for thinking on our feet?’" says Schmidt. "And that’s where, with COVID and this, it’s the firefighting of the moment. But there’s also a need to learn lessons for when this happens again and handle it better next time.”



