What to Know About the Current Avian Influenza Outbreak
Kathleen Hall Jamieson of the Annenberg Public Policy Center and Louise Moncla and Aliza Simeone of Penn Vet share helpful information for the public.

This story was originally published on Penn Today on October 16, 2024, and was updated on November 7, 2024.
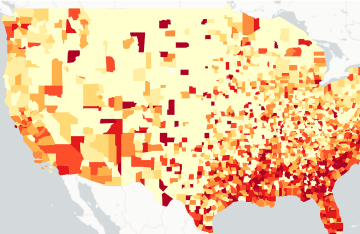
A Texas dairy herd first reported in March that cattle had tested positive for highly pathogenic avian influenza (HPAI). Since then, the H5N1 version of the virus has spread to 443 dairy herds in 14 states, according to the Centers for Disease Control and Prevention, which has also reported more than 105 million poultry affected in 48 states. Forty-six cases have been reported in humans this year.
“The risk of widespread transmission of avian influenza to humans is low,” says Cheryl Bettigole of the Department of Family Medicine and Community Health at Penn Medicine. “But we also know that agricultural workers, who work with cattle and other animals, are at highest risk of infection and that the majority of these workers are immigrants who have high rates of being uninsured.”
Louise Moncla, assistant professor of pathobiology at the School of Veterinary Medicine, notes that while human-to-human transmission of avian influenza has not been documented, there is some concern the virus could eventually evolve to transmit between people.
Bettigole moderated a virtual discussion about avian influenza featuring Moncla; Aliza Simeone, assistant professor of clinical infectious diseases and biosecurity at Penn Vet; and Kathleen Hall Jamieson, director of the Annenberg Public Policy Center in October. The Penn Center for Public Health held the seminar.
How did we get here?
Simeone explained that in 1983-84, Pennsylvania suffered an intense outbreak of the H5N2 subtype in poultry, resulting in the loss of one-third of the state’s egg production, $65 million in losses, and the activation of the National Guard. But this set the Keystone State on a path of preparedness decades before other states, and Pennsylvania has three testing labs, including one at Penn Vet’s New Bolton Center.
The H5N1 subtype was first identified in farmed birds in China in 1996. Moncla said these viruses historically circulated in domestic poultry populations in China, Southeast Asia, and northern Africa, Moncla said, but detections in Europe and then the Americas have increased in recent years.
The Moncla lab has been interested in trying to understand how the virus was introduced into North America and what has driven transmission, and researchers tackle these questions using viral genomics. One thing they learned was that the virus was introduced eight separate times, but the seven introductions from Asia didn’t take off. Most transmission stems from a single introduction from Europe.
What makes this different from past outbreaks?
Moncla notes that culling domestic animals from a flock effectively controlled a 2015 avian influenza outbreak in the United States. This was indicative of the transient nature of outbreaks, but that changed when viruses were detected in wild and domestic birds in Newfoundland, Canada, in late 2021. Since then, the viruses have become continuously present.
The way to adapt, Simeone said, is having more effective biosecurity measures to protect domestic poultry from wild birds. Simeone said Pennsylvania lost more than 4 million birds from the virus or from depopulation to prevent further spread, but this is still smaller than in the 1980s outbreak, due to improved surveillance and testing capacity.
Another change, Moncla said, is that infections from this outbreak have spread beyond the usual suspects of ducks, geese, and swans to scavengers, raptors, cranes, blackbirds, and songbirds. Her lab learned that the wild migratory birds are driving transmission, and therefore “we don’t need to start telling people to worry about healthy looking songbirds at their bird feeder,” she said. The outbreak has also spread farther and faster than previous ones, and it has been infecting mammals at a higher rate than previous ones.
“This outbreak has been really surprising because until this happened we had never known that cows had ever been knowingly infected with an influenza A virus, let alone a high-path avian influenza,” she said.
How can people protect themselves and their animals?
Reflecting on the aversion many had to masking and vaccinating during the COVID-19 pandemic, Jamieson said that assumptions had been incubating and were not knocked down sufficiently prior to the pandemic. With avian influenza, she wants to knock down misinformation proactively, in the event of a scenario in which it becomes transmissible from human to human and leads to a pandemic.
Specifically, Jamieson focused on raw milk. Simeone had noted she has seen more cats getting sick and dying at infected dairies because of raw milk exposure, whereas cat infections used to just come from exposure to infected poultry or wild birds.
“We know that the virus is in raw milk, and we know that raw milk isn’t as safe to drink as pasteurized milk, regardless of whether you think there’s any risk from HPAI H5N1,” Jamieson said, adding that there is a small but strong community that believes raw milk is better than pasteurized milk. She pointed to an Annenberg Public Policy Center survey conducted this spring which found that only 47% of respondents knew that raw milk is less safe to drink whereas others weren’t sure, thought it was just as safe to drink, or thought it was safer.
“You now see a partisan identity attached to a set of arguments that has raw milk within it,” Jamieson said. “That’s potentially worrisome in an environment where you have that level of public uncertainty about whether pasteurization is good or pasteurization is harmful.”
Recommendations from the panel included:
- Getting a flu shot
- Being careful when handling dead birds
- Acquiring more information by consulting federal agencies, such as dashboards from the U.S. Department of Agriculture, USDA information on protecting chickens, and risk reports from the CDC and World Health Organization.